Nepal offers some of the most sought-after trekking routes in the world. However, with the excitement of touching the clouds on treks like Everest base camp or Annapurna Base Camp, we often forget how high altitude sickness can affect trekkers and climbers.
With thousands of Nepalese nationals and foreigners bidding to reach some of the highest places on earth, there are serious risks of high altitude sickness associated with it. As the trekking routes in Nepal continue to become more accessible by road and vehicle, there has been an influx of high altitude related health issues.
Would be trekkers and mountain climbers in Nepal, without proper experience and knowledge of altitude sickness, poses a challenge for the medical teams working to keep them safe. With approximately 200,000 trekkers visiting Nepal in 2019 (Pre Covid-19), the task of being well stocked and prepared for emergencies has proven to be difficult for physicians in Nepal.
Interested in getting an idea of what High Altitude Sickness looks like? Watch one of the 7 movies about Everest we recommend!
What is high altitude sickness?
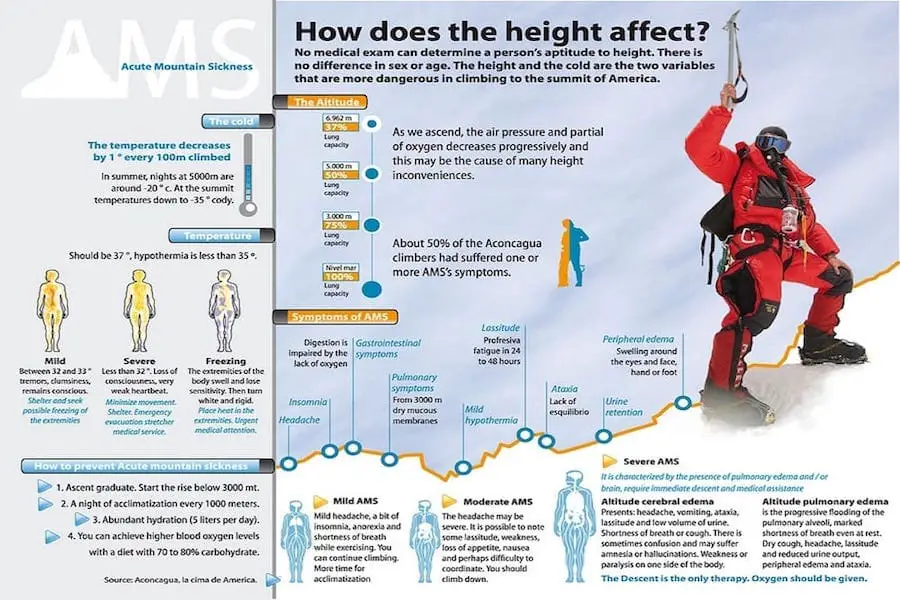
High altitude sickness happens when someone travels to high altitudes too quickly. More specifically, it can occur when trekkers above 2500 meters attempt to exceed 300-500 meters of sleeping altitude per day. Additionally, when a rest day isn’t taken after ascending 1000-1200 meters during the climb, AMS may set in.
There are three different forms of high altitude sickness, which all vary in severity. The next section covers the three types in more depth.
What are the different types of high altitude sickness?
High Altitude sickness is comprised of three different types of illness, with reversible Acute Mountain Sickness being the first form (AMS), followed by potentially fatal forms of illnesses known as High Altitude Cerebral Edema (HACE) and High Altitude Pulmonary Edema (HAPE).
AMS is a common form of altitude sickness and is prevalent in approximately 60-70 percent of travelers ascending to altitudes greater than 2,500 m, while HACE and HAPE are less common, affecting only 1-2 percent of travelers. They tend to be less common because trekkers usually take note of the first stages of Acute Mountain Sickness, and then take the necessary precautions to protect themselves.
The various mechanisms behind these three types of high altitude sickness are not completely understood and the prevalence of them is highly variable among individuals and even more so amongst various ethnic populations (think the high altitude populations living in the Himalayan Ranges like Sherpas or Tamangs). Moreover, depending on the individual, they may be able to acclimatize better or even be more resistant to altitude sickness in general.
As altitude increases the partial pressure of oxygen in the atmosphere is reduced, this is known as hypobaric hypoxia. This means that the body is deprived of a sufficient supply of oxygen from the air to supply for body tissues. Once exposed to this issue the body begins to work to acclimatize itself to the reduction of oxygen pressure at high altitudes in order to maintain functionality.
A few ways the body is able to handle these changes is by increasing its breathing rate and heart rate as well as kidney functionality and urine production. The body will work to acclimatize itself to handle its new environment during the short term. However, eventually the body will begin producing more red blood cells in order to transport more oxygen to help acclimatize itself to live at high altitudes for longterm.
High Altitude Sickness as resulted in people dying on Everest – some of which are still frozen on the mountain. Read about Death on Everest – and the 200 bodies still frozen in the death zone.
When does high altitude sickness happen?
Acute Mountain Sickness occurs when trekkers reach to 2500 meters and above, and attempt to exceed more than 300 to 500 meters of sleeping altitude per day. Additionally, when a rest day isn’t taken after ascending 1000-1200 meters during the climb, AMS may set in.
Trekkers may further be affected by AMS when they become dehydrated, overexerted or are not properly protected from the cold and hyperthermia. Therefore it is recommended that climbers use rest days, don’t exceed 500 meters in sleeping altitude change in a day, stay hydrated, be cautious of their abilities and not over exert themselves. Moreover, there are prophylaxis for altitude sickness like Acetazolamide (Diamox) but these should only be used after consulting a doctor first!
What are altitude sickness symptoms?
The symptoms of AMS vary from individual to individual, with mild to moderate symptoms including: difficulty sleeping; dizziness; fatigue; headache; loss of appetite; vomiting; shortness of breath; and, rapid pulse.
Symptoms of HACE as well as HAPE are more severe and immediate medical attention should be found. They include: blue color to the skin (cyanosis); chest tightness or congestion; confusion; coughing up blood; decreased consciousness; gray or pale complexion; cannot walk in a straight line, or walk at all; and fluid or swelling in the brain.
Treatment of high altitude sickness
The main treatment for altitude related illnesses and especially with Acute Mountain Sickness is to simply move to a lower altitude. However if the trekker has a more severe condition of altitude sickness like HACE or HAPE, the Cleveland Clinic from the United States has cited the following treatments:
- For fluid in the brain (HACE): you may need dexamethasone, a steroid that helps reduce swelling in the brain. Dexamethasone is sometimes prescribed as a preventive medication.
- For fluid in the lungs (HAPE): you may need oxygen, medication, a lung inhaler or, in severe cases, a respirator.
- If you need more oxygen: a provider might prescribe acetazolamide, which increases your breathing rate, so you take in more oxygen. The medicine helps your body adjust faster to the higher elevation and reduces symptoms of altitude sickness.
Getting trekking insurance, can be one of the best ways to protect yourself while climbing to high elevations. Many trekking insurance providers will cover the expense for emergency medical evacuation if you succumb to altitude sickness.
Curious about the elevation in different parts of Nepal? Then check out my blog that covers the elevation of Kathmandu and other major cities in Nepal!
Why is high altitude sickness a problem in Nepal?
According to Himalayan Rescue, on average there is one death out of every 30,000 trekkers in Nepal due to high altitude sickness related complications each year. Moreover, Himalayan Rescue states that deaths related to high altitude have been falling over the years, but the deaths are still too many as they are completely preventable with proper knowledge and care.
Dr. Santosh Baniya, a MDGP and Emergency Physician, as well as a team member of the Mountain Medicine Society of Nepal, discussed a few other reasons why there are issues with high altitude sickness in Nepal. Whereas, in a Medicos Next interview, he discussed the rising issues around alcohol consumption while trekking and the increased access to direct flights to high altitude areas, as well as roads that are reaching high altitudes allowing for increased access by vehicles, in areas such as Manang.
Re-entry High Altitude Pulmonary Edema:
The quick and easy access to high altitude areas in Nepal has led to the development of a relatively new illness in Nepal. Known as Re-entry High Altitude Pulmonary Edema. Although not unique to Nepal, as it is a common phenomenon in South American Andes, it has been growing in prevalence in Nepal as of late.
The issue is not as much as with the illness but the lack of knowledge among physicians and Nepalis. Moreover, Re-entry High Altitude Pulmonary Edema has become prevalent recently with Nepalis living in high altitudes for most of the year in areas like: Lake Tilcho (4,900 m) and Lake Gosaikunda (4,380 m).
With road access increasing in these two areas, Nepalis living in the regions have been able to drive to low elevations and back during the off seasons as well as to get supplies when needed, and then returning quickly to their homes at extreme altitudes. Resulting in an increased number of Nepalis contracting Re-entry high altitude pulmonary edema or other severe forms of altitude sickness like High Altitude Cerebral Edema and High Altitude Pulmonary Edema.
Nepal’s rescue and aid posts for trekkers:

Luckily, if you are trekking in Nepal, and begin to feel signs of high altitude sickness, Nepal has well-established rescue and aid posts throughout the Annapurna and Everest region. A few of the post locations include:
- Pherice (4,300 m)
- Everest Base Camp (5,300 m)
- Manang (3,500 m)
- Machhermo (4,410 m)
- Gokyo (4,880 m).
High Altitude Sickness – Protect yourself while trekking
No matter where you are trekking in the world it is important to be aware and knowledgeable of the symptoms of high altitude sickness. As treatment and response continues to get better in Nepal, trekkers will continue to have a safer time while trekking the tallest mountains in Nepal.
However, as noted by Dr. Santosh, it is important that we as trekkers take the precautionary steps to keeping ourselves safe. This means monitoring our own health, educating ourselves about high-altitude sickness, keeping alcohol consumption down while trekking and climbing, as well as taking the proper rest days when needed.
Finally, the most important thing to remember is that no one is immune to high altitude sickness. No matter your genetics and previous accomplishments.
